- Locally, the treatment gap for Indonesia for psychosis is the highest at 96.5% among developing countries.
- According to Indonesia’s 2007 Demography and Health Survey, 11.6 percent of people, 15 years old and above, experienced minor mental health problems such as anxiety and depression while 0.46 percent of the total population of the country experienced serious depression, such as manic depression or schizophrenia (The Jakarta Post, 2011).
- An estimated 1.1 million Indonesians suffers from serious and chronic mental health issues. Yet only 0.023% of the 2011 Indonesian budget is spent on mental health, given that the health budget accounted for only 2.3% of the total national budget (Suarez, 2011).
- It is no wonder that there is a severe shortage of mental health services. In a country of almost 240 million people, there are only about 800 psychiatrists out of the recommended 8,000 (if the ratio of 1 psychiatrist : 100,000 population is kept), implying a shortage of 90% (WHO, 2011; The Jakarta Post, 2011)!
- There are 48 mental hospitals with more than half of these psychiatric hospitals located in four out of 34 provinces. Eight provinces does not have psychiatric hospitals to date.
- The unequal distribution of mental health services, with concentration in big cities like Jakarta and Surabaya, meant that there is an inherent structural difficulty in access for persons with mental illness(es). Most do not get the services they require and families resort to restraining their children as a result.
- The phenomenon of pasung has gained the attention of Human Rights Watch and is considered a severe violation of human rights. In 2014, the Mental Health Law was passed, emphasising that “treatments for mentally ill people should ‘provide protection and guarantee services’ and ensure no human rights violations in the process (Jakarta Globe, 2014).”
- It may still be a long process before most persons with mental illness(es) get treated in Indonesia but the law has created momentum for “Bebas Pasung” the freeing of persons with mental illness(es) who are chained. This is a good sign.
A study undertaken to consider the perceptions of Indonesians living in Yogyakarta towards persons with mental illness(es).
Sunday, November 22, 2015
Indonesia's Mental Health Landscape
Comparison of Mental Health Capacity of Southeast Asian Nations
Regionally, mental health has been a low priority. In most of the Southeast Asian countries, “mental health spending is no more than 2% of the health budget, with 80 - 90% going to mental hospitals.” Poor mental health has also been linked to slower development. “The direct consequences of neglect are many, including avoidable disability, impoverishment, and widespread human-rights abuses (in the region).” A comparison of the mental health capacity across Southeast Asian nations can be found in the Table above (Maramis, Van Tuan & Minas, 2011).
Perceived Barriers to Help-Seeking: Perceived Stigma, Poor Mental Health Literacy and Lack of awareness on places to seek help
What are the perceived barriers towards help-seeking in Yogyakarta among youths?
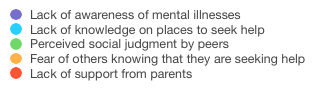
According to the youths surveyed, the top five barriers towards help-seeking are (1) lack of
awareness of mental illness (61.8% - 131 respondents), (2) lack of knowledge on places to seek help
(52.8% - 112 respondents), (3) perceived social judgement by peers (48.6% - 103 respondents), (4)
fear of others knowing that they are seeking help (40.1% - 85 respondents) and the (5) lack of
support from parents (32.1% - 68 respondents).
Perceived barriers -- across cultures
|
|
Comparisons across culture
|
|||
|
|
|
WESTERN
|
SINGAPORE
|
YOGYAKARTA
|
|
1
|
Barriers to help-seeking
|
Lack of a perceived need for help
|
Fear of Peer Stigma
|
Lack of awareness
|
|
2
|
Lack of awareness of services or insurance coverage
|
Lack of information on where to seek help
|
Lack of knowledge on were to seek help
|
|
|
3
|
Scepticism — perceived ineffectiveness of treatment programme
|
Lack of time
|
Perceived social judgement by peers — fear of peer stigma
|
|
|
4
|
Religious prohibition and discouragement
|
Parents do not encourage help-seeking
|
Fear of others knowing
|
|
|
5
|
|
Fear that conditions will not be kept confidential by schools
|
Lack of support from parents
|
|
- A comparison across three cultural contexts of Western, Singapore4 and Yogyakarta, revealed that the factors of perceived stigma, poor mental health literacy and lack of awareness on places to seek help, consistently surfaced as key barriers towards help-seeking.
- This finding has implications on the prioritisation of mental health promotion, prevention and engagement efforts, when tackling barriers.
- Strategies for improving help-seeking for youths should focus on reducing perceived stigma by debunking myths and abating concerns that others will judge, improving mental health literacy and in raising awareness of the public on places offering mental health services.
Saturday, November 7, 2015
Let's build a mentally healthy generation (7/11)
[7 NOV 2015] SEMINAR SOSIALIASI KESEHATAN JIWA “MENYIAPKAN GENERASI SEHAT JIWA SEJAK DINI” @ RSJ GRHASIA DIY
Observation
- lack of appreciation shown via a lack of clapping at seminars
- leaving things behind for others to clear
- need to have an official opening
- Only 12 out of 80 in attendance are males
- It is interesting to see what psychologist Dr. Adiyanti classify as problems and strengths of youths
- Spirituality is a major component of mental health in Indonesia
- Definition of “what does it mean to have a mentally healthy generation?”
- Creating a generation that is not free from all problems but one that can solve their own problems
- Dr. Ida: Attribution of causes to B.P.S., when do we need to bring the kid to the professional?
#aib = #stigma
#attributionofcauses
#discipliningofunreasonbyreason
| Dr. Maria Adiyanti | What will you prioritise as the issues to resolve for children and youths? |
| Dr. Astriana Praharani, Sp.A, Child Specialist |
What do people in the community usually attribute as the causes of mental illnesses? |
KESWAMAS
- focus on promotion and prevention
Mbak Tyas’s speech:
- over social media, we have seen cases of cyber-bullying
- this world we are living in, has many influences
- challenges for raising and educating kids
Audience
- Dinas Kesehatan Kabupaten — healthcare policymakers
- TK (kindergarten) teachers
- Healthcare Professionals
Head, RSJ Grhasia
- “We need to go close to the community, the mental health hospital cannot just stay in the institution. We need to have efforts that focus on promotion and prevention. That’s why KESWAMAS was started.”
dr. Astriana Praharani, Sp.A, Child Specialist
- growth stages of children
MENCIPTAKAN GENERASI SEHAT JIWA (CREATING A MENTALLY HEALTHY GENERATION)
Dr. MG. Adiyanti
Just like cooking “nasi goreng,” the taste cooked by different people always come out different. Even though, the ingredients added and climate might be similar. Nurturing kids and youths are not that much different.
Some problems
- hooked on to phones
- depression by loneliness / neglect / bullying
- child abuse
- cyber bullying
- bullying in school
- lack of aspirations
- free sex
- pre-martial sex and closeness
- heavy smoking
- glue sniffing (even for kids) and drugs
- abortions
Some strengths
- people dedicated to the promotion and participation of arts and culture
- participation in competititons, bringing glory
- participation in KKN
- working to provide for family
- participation in discussions for academic improvements
The double-lives of youths
- religiousity — pray 5 times a day
- but take drugs 5 times a day too
- and say as long as he don’t get caught, he will continue
What does it mean to have a mentally health generation?
- A generation that is not only physically healthy, but also psychologically and spiritually
- sebagai generasi yang sehat baik fisik, psikis maupun rohani
- Generation
- not a generation that is free from all problems
- but a generation that can solve their own problems by their own means
- people who can be accepted by their neighbourhood
- people who do not causes harm to others
- people who do not hurt themselves
Contribution
- organic
- supervision
- by teachers and parents
- interpersonal
- intrapersonal
- socioeconomic status
The conditions are different
- technologically savvy
- connected generation
- information-bombarded generation
“It takes a village to raise a child.” — African Proverb, popularised by Hillary Clinton
The village in Yogyakarta, Indonesia consists of:
- Playgroup (TK)
- Sessions for kids to read the koran
- Plays for learn-n-play
- Scouts
- Pendidikan Anak Usia Dini - early childhood education programmes
- Summer camp adventure club
Strategies
- give kids money to shop but give rules — learn skills of financial planning, budgeting
Kid get bullied but dare not say out of threats.
- How will parents / teachers resolve this problem?
- Kids solved their own problem:
- teacher ask what can you all do?
- the kids thought and said we can accompany each other
- safety in company
Thinking out of the box
Mengenal dan Mengelola Kesehtan Jiwa pada anak dan remaja
Dr. Ida Rochmawati M.Sc. Sp. KJ (K) RSUD Wonosari Gunung Kidul
Problems
- what does it mean to be “naughty” for kids?
- could it be attention-deficit disorder? or ADHD instead?
- Social training — whose role is it? — a prevalent perception of females below males?
Why is it important for us to talk about mental health in Yogyakarta?
- Berdasarkan hasil Riset Kesehatan Dasar (RISKEDAS) 2007 prosentase gangguan mental emosional mencapai, 11.6% dari sekitar 19 juta penduduk yang berusia 15 tahun ke atas
- Based on the results of Basic Health Research in 2007 the percentage of mental disorders emotional reach, 11.6% of the approximately 19 million people aged 15 years and over
What are the common mental health conditions?
- Cemas pada anak (anxiety)
- usually expressed through physical reactions (inability to relax, always falling sick, headache)
- affective disturbance — depression
- gangguan perilaku (disturbed behaviour)
- eating disorders
- PICA
- Anorexia
- Bulimia
- elimination disorders
- Enueresis
- psychosis
- Autism
- Mental retardation
Insomnia (types)
- broken insomnia — usually depression
- insomnia alone — usually anxiety
- insomnia — can sleep but wake up early and can’t return to sleep
Apa penyebab dari gangguan jiwa? (What causes mental disorders?)
- Biological
- Psychological
- Social
Stigma
- erroneous perceptions from the community
- it delays help-seeking behaviour
- because of erroneous attribution of problems — not to BPS
Monday, October 19, 2015
Wednesday, October 14, 2015
Lecturer Pak Koentjoro: "Mental health is harmony!" (15/10)
Friday, October 9, 2015
Perceptions towards ODS & Integration (How) (9/10)
Perceptions towards ODS & Integration (How)
What is it shaped by?
- exposure to media
TV (electronic)
Print (newspaper and magazines)
- family's reactions
According to Pak Harry
- some call them "gila"
- some see them as "lucu" - a laughing joke
- others make fun of them and see them as source of amusement
Stigma exists among neighbours and friends.
How can we achieve integration?
Systemic (Mbak Aspi)
Devotion of more Economic resources
As an individual, shift in mindset
- we can learn more
- we need to stop seeing them as not normal - and other-ing them
- it's true that they are sick (illness)
- we can and must see their assets and appreciate their ability to do small tasks
For caregivers
- help them care for ODS
- enable them to educate others - share their story with others
- support others
Caregiver felt alone and not understood (9/10)
Mas Agus and Cousin (Caregiver and ODS) (9/10)
Mas Agus has a Cousin diagnosed with schizophrenia
Mas Agus has a Cousin diagnosed with schizophrenia
First time when he knew that his Cousin got diagnosed
- he felt alone
- no one understand
- inferior - didn't want to invite friends back home
- "why ODS in my home?" - questions why does it have to happen in his home?
- over time, he said his family comes to realise that he is STILL family
- even though he is different from "orang Biasa"
How do others react?
- "takut"
- "Sakit"
Caregiver's Journey: Relapses are common, Managing Reactions of neighbours (9/10)
Pak Harry and Son (Caregiver and ODS) (9/10)
Pak Yustinus Harry Nugroho and his Son who was diagnosed with schizophrenia
He started his sharing by showcasing the behaviour of his son, smoking non-stop, looking aimlessly and talking to self.
Pak Yustinus Harry Nugroho and his Son who was diagnosed with schizophrenia
He started his sharing by showcasing the behaviour of his son, smoking non-stop, looking aimlessly and talking to self.
Reactions to diagnosis
When he was diagnosed, he will keep asking "why can't I go university?" He will punch himself.
#Evidence of self-blame via self-punishment.
During a relapse:
He talked to himself.
Prayed to "nobody"
Chain-smoked
His eyes were empty.
He will walk on his own - "kosong"
#Relapses are common.
How he felt
I felt really sad (sedih sekali)
Why must it be my Son?
How he react?
@Neighbours
- not defensive
- patient, explain to them, help them understand
(I received encouragement from the Neighbours in my Neighbourhood, many well wishes that he can become better)
Harus optimise. Harus positive!
What helped Pak Harry
Attended a training for caregiver by RSJ Grahsia
- he received social support
- realised that he is not alone
- became convinced that there is hope for recovery for ODS
He now runs the support group independently.
He now runs the support group independently.
He wished for:
- more community support
- more understanding and empathy towards PMI
Recorded post-seminar on "Undersranding Schizophrenia" Organised by Lembaga Mahasiswa Psikologi on 9 October 2015
Saturday, September 26, 2015
Operationalising the construct of Perceptions
Perceptions: Association, Attribution, Reactions
My Questions to Mental Health Professionals:
My Questions to Mental Health Professionals:
Attribution: why? - what's the cause?
Treatment: how?
Reaction:
- mental health landscape (what's good / what's lacking?)
- spiritual treatment (dukun / kiyai) - possibility of partnership?
- stigma?
- Javanese cultural factors that act as protective factors?
- patients reaction to diagnosis?
- caregivers?
- community's reaction?
Association:
First word?
Saturday, September 19, 2015
Associations: Words Used to describe persons with mental illness(es)
Technique to operationalise "Perceptions"
* Association
* Attribution (meaning)
* Reactions
What people in masyarkat say about PMI (19/9)
- gila - anyone who enter must be crazy
- Sinting - gila
- kenthir - gila
- gemblung - people who are very stupid
- stress - when one has too much, it affects one's ability to think straight
Results of survey
Results of survey
Kasihan (pity)! My research surfaced kasihan (pity) as the
most common word associated with
persons with mental illness(es) where
more than 40 respondents out of 200
(20%) cited this as the first word that
comes to mind when thinking of such
persons.
Besides kasihan (pity) other words commonly associated (Chart 1) are gila (crazy) — 12.5% (25 respondents), sakit (sick) — 7.5% (15 respondents), edan (crazy), aneh (weird), kucel (crumpled), berbeda (different), kosong (empty), hilang (lost) and Islamic proclamations: astagfirullah (forgiveness from Allah), innalillahiwainailaihirojiun (surely we belong to Allah and to Him shall we return).
Besides kasihan (pity) other words commonly associated (Chart 1) are gila (crazy) — 12.5% (25 respondents), sakit (sick) — 7.5% (15 respondents), edan (crazy), aneh (weird), kucel (crumpled), berbeda (different), kosong (empty), hilang (lost) and Islamic proclamations: astagfirullah (forgiveness from Allah), innalillahiwainailaihirojiun (surely we belong to Allah and to Him shall we return).
RSJ Grahsia: Learning from experienced mental health professional Mbak Aspi (19/9)
RSJ Grahsia (observations on environment)
- tenang (peaceful) on Sat
- focus on rehabilitation
- located far from city centre (usually for rehabilitation houses)
- bureaucratic - requires letter from Heads to Heads - shows the importance RSJ Grahsia placed on patients' confidentiality
Interview with Mbak Apsi of KESWAMA revealed:
- menolong - PMI can be helped and more can be done to help them. I want to do what I can to help them.
- there are barriers - due to bureaucracy - challenging to go directly to people - the stratified hierarchy suggest that there are levels to go - this might incur inefficiencies - as evidenced by the result of DSSJ being spread to 6 villages in 5 years
- DSSJ (Desa Siaga Sakit Jiwa) - Village Readiness for Mental Illness - is a Programme targets at 5 regencies in D.I.Y.
- patients that come to Grahsia from the desa (village) are usually those who have gone to the dukun for 5 to 10 times with no results
- the families usually have huge debts and lost many savings at this point in time (bcoz the demands of ube rampe from a dukun can be extremely challenging to attain) - desperate to help their kids
- Grahsia is usually seen as the last choice to go to - the last resort
- not really possible to work with dukun because
(1) medical practitioners see them as being of lower status (dislike to associate) - no evidence / non-scientific
(2) agama - musyrik is not good - everything is planned by God - nrimo better
(3) because of stigma, dukun many times don't identify themselves as dukun - they call themselves kiyai, religious leaders who are experts on paranormal phenomenon
- Going Forward: How can we achieve better mental wellness?
* research
* sosialisasi (psychoeducation promotion and training)
* bebas (free) pasung movement - and treat them medically and with dignity
* reduce stigma through education
* build connections between sectors
Remark by Anita, S2 senior
(it is better to be possessed than to be mentally ill)
Friday, September 18, 2015
Ojek Pak Yanto's experiences with PMI (19/9)
When I shared with Pak Yanto that I will be visiting RSJ Grahsia today, he shared with me his experiences.
The Area
He passed by that area frequently to visit his Friend and send people to a park near there. He said there are many "orang gila" in there. Outside, there are a few. Sometimes, they are thrown out because they do not have money to pay since their family had abandoned them after some time.
Experiences with PMI @ Security Post - what they asked for
When he was working as a security guard, he recounted that there was this man who always come to where he work. He will ask for food (Nasi goreng). After which, ask for drink (Es Teh). After which, ask for cigarettes. Pak Yanto said he will buy them and give it to him. He said the man seldom talk to others, even though he's gila. But according to Pak Yanto, he seem to trust Pak, so Pak Yanto, will help him when he ask. Pak said the man used to be a mahasiswa until stress proved too much to take.
University students' stress in kota pelajar?
A Friend who died
Pak Yanto said he had a Friend who had problems with his thinking. Especially when the weather gets hot. He will show signs of distress and become angry easily. He will often ask food, drinks and cigarettes from Pak. He didn't used to be like that. Passed away recently.
Pak's attributions of expressions of anger as a mark of PMI
On the way x4
Pak Yanto pointed out to me 4 times on my 15 minutes journey from my rumah kos to UGM's library, people on the streets who he claims are orang gila.
There was a man who looks decently dressed but was hunched over sitting along the pavement with his head buried, under the hot sun.
There was a "mahasiswa" (young) according to Pak, along the street talking to himself.
There was a woman (presumably in her 50s) who was dressed in clothes that were a little tattered and torn. She was toying with garbage and had a bicycle beside her loaded at the sides with plastic bags full of "garbage".
Appearance - untidy
Signs - talking to self
Abnormal - sitting under the sun
Living around PMI
I asked Pak if there were orang gila in his community. He said yes! But the guy was often in his house, and does not disturb others. He said there are people in the community that doesn't like him. He's okay with him.
Peaceful co-existence? An uneasy peace? - rukun
Why did people not like him?
Monday, September 14, 2015
Peer Aulia: Religious fanaticism and ODGJ (14/9)
Aulia's sharing:
Religious fanaticism - phenomenon in Central Java
- fanaticism - prejudice - group polarisation
- Same Allah but different religious practices - clash in Central Java
On ODGJ
- first word: gangguan
- dukun for orang Desa (uneducated)
- people approach kyai too (but after consultation, just drink water, not psychiatric medicine) - opportunity for collaboration?
- she don't believe in dukun or kyai
- will recommend friend to seek psychological help should he/she exhibit symptoms
- perspective towards medicine?
Friday, September 11, 2015
[CPMH] What happens when you bring teachers, students and parents together?
What happens when you bring teachers, students and parents together?
This initiative, School of Wellbeing Training is a psycho-education workshop for the above stakeholders initiated by CPMH, MOE & MOH.
Guru
- The affirmation-exchange activity was profound!
- Parents teared! Fathers and mothers alike.
- Teachers smiled heartwarmingly.
This initiative, School of Wellbeing Training is a psycho-education workshop for the above stakeholders initiated by CPMH, MOE & MOH.
- The students are taught techniques to gain success via goal-setting and having dreams. They are also made to write affirmation notes for their parents and teachers.
- Teachers are taught to communicate with empathy to their students (techniques of empathic communication). They are also taught basic techniques of counselling and ways to spot problems among youths.
- Parents are taught communication techniques and the use of affirmations to nurture their children.
Guru
Meeting KPSI Yogyakarta's Founder Dr. TIKA (23/8): Nongkrong (hangout) with caregivers
Meet Dr Tika :)
She spends her Sunday morning today, cooking for and facilitating the sharing for Komunitas Peduli Skizofrenia Indonesia Jogja's caregivers and consumers together with her team.
I am so glad to finally meet Dr. Tika in person!
Via the practice of nongkrong - Dr. Tika is able to nurture a culture of support among caregivers, persons with mental illness(es) and professionals like herself.
Anthropologist Margaret Mead once said, "Never doubt that a small group of thoughtful, committed, citizens can change the world. Indeed, it is the only thing that ever has." Social change can happen with combined efforts. To feel supported, to be understood and to realise one is not alone, are human needs that while simple, is profound especially for persons struggling with mental health issues.
I look forward to learning more from her. Striving together towards a world where there's mental wellness for all :)
Thursday, September 10, 2015
#6 - Ojek knows PMIs (10/9)
Encounter with PMI (10/9)
It was 8 am and I was exiting from my rumah kos to take my Ojek (motorcycle taxi) to school. There was a man (in his late 50s) loitering outside my rumah kos, he looks lost. Just as I was boarding my Ojek, he asked me if I had seen his son from Jakarta inside my house. I replied no, and that I am sorry before boarding my Ojek. My usually talkative Ojek Pak Yanto was unusually quiet throughout this episode. As my Ojek moved, I close the main gate behind the man.
(Why did I do that? - was it out of fear?)
As we moved on, Pak Yanto said: "Dia orang gila!"
I asked, "Bagaimana Pak tahu?"
Pak Yanto: "Kelihatanya dia hilang. Pakaian kotor sekali ya."
Note to self
#Terms Of Address for PMI: Orang Gila
#Judging PMIs based on appearance - an appearance conscious Javanese
I asked "Ada banyak di Jogja?"
Pak Yanto: "Banyak! Terutama di Grhasia. Mau pergi ke sana? Kira-kira 15 menit."
I replied, "ya! Mungkin suatu hari ya."
Pak Yanto went on to share with me how they are followed by spirits (diikuti makhluk halus) and are possessed. Some are dangerous and have to be "tangkap." "Mungkin dia yang lalu, jahat."
I asked, can they recover (bisa sembuh?), according to him?
He said maybe.
I asked have he heard of terms like psychosis, schizophrenia and "gangguan jiwa". He said no.
Key Reflections
This encounter is revealing of perceptions of laymen in the community towards persons with mental illness(es). The labels and terms heaped upon them "orang gila" appears to be sweeping but telling of attitudes. The perception that " diikuti makhluk halus" suggests that mental illness(es) are still very much linked towards spiritual notions of possession and karma (Mungkin dia yang lalu, jahat). His silence at the start when the (lost) man was around, suggests a sense of avoidance and discomfort, yet his silence indicated that he wanted to maintain "rukun" (harmony) and not even engage, much less confront the man.
Wednesday, September 9, 2015
#5 Youths in Jogja: Dissonance, Adjustment and Illness?
Conversations with Mbak Wenty, internship supervisor on the state of youths in Jogja
More well-informed: access to more sources of information. More resources
As an educator, this is good as "discussions (among students and teachers) become richer."
- Mbak Wenty
What are some issues of concern?
Students might feel overwhelmed by the wealth of information.
This information can be used for good and bad. Exposure to media - advertisements inspire wants and consumption. Lifestyle choices like pornography and free sex may be influenced.
There are concerns with emotional well-being of students. Tensions between the desire for pre-marital sex and religious fundamentalism (a return to more religious piety). Some lead double lives. Mental stress and guilt may occur as a result.
Adjustment issues. This is compounded and complemented with the fact that in Kota Pelajar, many students are away from home and realise their newfound independence endows them with power to make decisions independently and choose what lifestyle they want.
These decisions can go a long way in influencing their future and outlook.
Dating culture
Pre-dating is usually done via social media and LINE rather than in person. Dating is before and after getting into a relationship in Singapore. But in Indonesia, dating is done after the guy ask the lady to be his pacar, with the preparation/intention to get married.
According to Luthfi, Undergraduate (Law), these are the youths problems of the day:
- free sex
- drugs
- ethics (cheating, plagiarism, corruption - bribing)
These "sins" and lifestyle choices can lead to the development of "ill" mental health.
#4 Medicalising / Diagnosing Mental Illness(es) via DSM-IV
The dominance of the medical model (9/9)
Tuesday, September 8, 2015
#3 - PMI: How can I get help?
Conversations with Supervisor Mbak Ariana, M.Sci Social Work - Week 2
This is a map of the "defences" in the system.
For those in the community / the poor without private insurance, they have to go to PUSKEMAS first. If they need specialist treatment, they must get a referral. Similar to the Polyclinic system in Singapore.
#1 - Primary Health Care - PUSKEMAS
(for those with General Insurance Coverage)
#2 - Secondary Health Care - hospitals
(For those with private health care insurance)
Reminder: learn about the city structure
Key reflections:
Mbak Ariana related those who sought the help of dukun as those who are less educated and those who have less access to services.
How can we improve the mental health services?
Mbak Ariana wishes that more districts have psychologists. The alternative is to have more GPs and nurses trained in mental health. The current issue is there is a limited supply of psychiatrists and psychologists.
Eg. Community Mental Health Nurse (CMHN) programme - to train and certify nurses
Eg. GP+ programme - qualify GPs to do assessments and prescribe anti-depressants as well as anti-psychotics
Eg. Targeting the community to support PUSKEMAS
CPMH has a new initiative to train volunteers in mental health - mental health cadre. They will help to conduct initial screening for PMIs, deliver psychoeducation but NOT interventions.
Referred me to Mbak Nurul, who's heading the initiative. Will get involved in the planning for the training which will happen in 2 weeks time.
Thursday, August 20, 2015
Resources: Peers and Professionals - What I learnt from them
PEERS
- Iconx - UGM FoP Graduate - Valedictorian, Peer in Recovery
- Explained concept of Rukun (harmony) to me
- Swastaji Agung Rahmadi - UGM IR, Junior Researcher, Indigenous Javanese in Yogyakarta
- Indigenous concepts are important to understand Javanese in Yogyakarta
- Afina - UGM IR
- Terms commonly used to refer to persons with mental illness(es) like idiot, autis, gila has seeped into daily language.
- Peers at PSSAT
- Peers at Korean Language Diploma class
- Peers at CICP, Faculty of Psychology, UGM
- Aliya helped me with the translation of my survey from English to Bahasa Indonesia.
PROFESSIONALS
- Mbak Ariana - CPMH MSW
- Suggested that I used a quantitative approach.
- Supervisors Dr. Wenty - youth specialist
- Encouraged me to use mixed methods, combining ethnographic observations, with qualitative interviews and quantitative findings.
- Mbak Aspi - Community Mental Health Worker at RSJ Grhasia (KESWAMAS), former psychiatric nurse, current Masters candidate at UGM Faculty of Psychology
- Exposed me to various phenomenon
- Training of housewives - mental health cadres in the villages x 2 for "Empathic Communication - Basic Counselling"
- Caregiver Support Group for persons caring for persons with mental illness(es)
- Talks on "Understanding Schizophrenia", "Creating a mentally healthy generation," and "Overcoming Stigma in Yogyakarta"
- Pasung of Luji Lestari
- Ibu Tyas - Chief Community Mental Health Worker at RSJ Grhasia (KESWAMAS), former psychiatric nurse
- The stigma mental health professionals faced from their own families
- Mas Tarjo - Community Mental Health Worker at RSJ Grhasia (KESWAMAS), former psychiatric nurse
- Pasung
- Psychiatrist - Dr. Ida Rochmawati
- Global, national and local view of the state of mental health in Yogyakarta
- Media plays a negative role of perpetuating stigma (because their focus is on news angle)
- Psychiatrist - Dr. Tika Prasetiawati
- Media plays a dual role -- perpetuating stigma and educating communities positively
- Psychology Lecturer - Pak Subandi, Vice Dean Faculty of Psychology
- Spirituality is central towards wellness and illness.
- Psychology Lecturer - Pak Koentjoro, Expert in Community Development
- Indigenous concepts of happiness are key to wellness - this can be done through Ki Ageng Suryomentaram's teachings - indigenous psychoanalytic approach to happiness
- Ibu Emmy, Laughter Yoga Teacher
- Laughing without reason may be perceived as "crazy" but laughing without reason is also the key reason to train our mind via behaviour to inspire paradigm shifts to induce happiness!
Thursday, July 23, 2015
#1 - "How can I be normal again?"
#1 - Pre-Exchange - Pak Bambang's story - Memory of my face
Pak Bambang asks, "how can I be a normal person again?" Something fundamental yet profound. What does it mean to be normal?
Bambang Rudjito is a university-educated Indonesian man diagnosed with schizoaffective disorder with a caring wife and energetic son.
In his words, "Mental illness is just like any other illness, if the doctor says that you have to take the medicine, do take it. Don't stigmatize the family. Please be there and support the patient so he feels good about himself, and gets better and recovers. ... Please be aware and admit that we are ill, because from the awareness that we are ill will emerge the intention to recover and to be better and better, to get better and better." - Bambang Rudjito
Powerful storytelling through the lenses of a person afflicted with mental illness.
Subscribe to:
Posts (Atom)